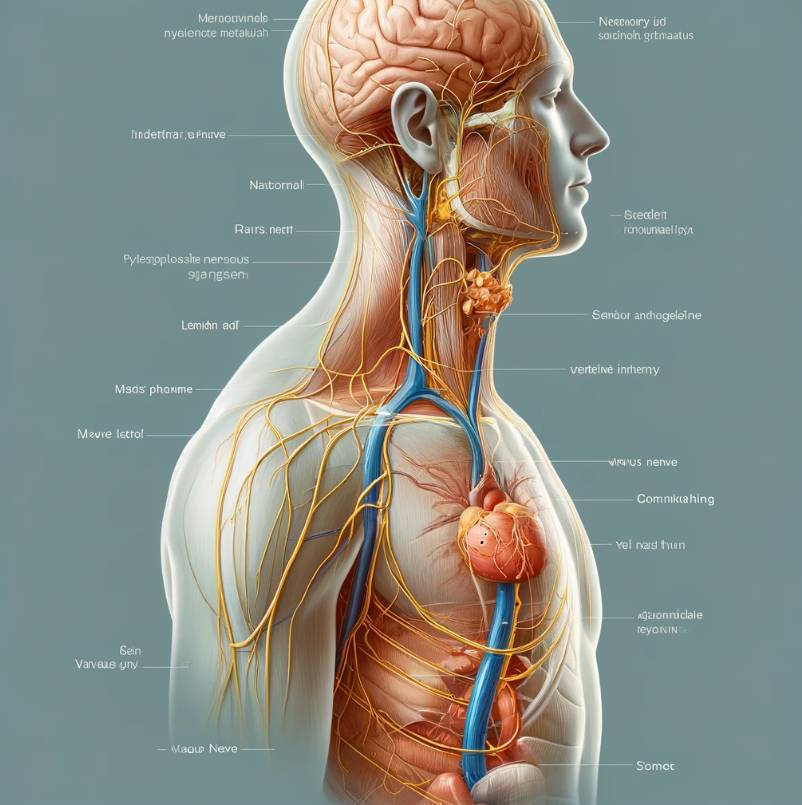
Vagus nerve stimulation (VNS) therapy has proven to be transformative for patients with drug-resistant epilepsy and is gaining traction in other indications, including treatment-resistant depression (1). It typically requires a vagal nerve stimulator to be implanted under the skin in the chest area, which then transmits electrical stimulation to the vagus nerve. As the use of this therapy expands, it is critical to have a comprehensive understanding of the impacts of a vagal nerve stimulator on surgery safety and outcomes.
In the preoperative phase, a thorough review of the patient’s medical and surgical history is essential. This evaluation should include an assessment of the patient’s response to VNS, taking into account the frequency and severity of any seizures or depressive episodes, and noting any side effects of VNS therapy. Additionally, it is important to identify the type of VNS device implanted, its settings, and the last date of maintenance or adjustment. A vagal nerve stimulator can affect cardiac function and interact with anesthetic drugs administered during surgery, which can lead to complications such as bradyarrhythmias and other impacts on safety. These challenges require anesthesiologists and neurologists to carefully consider whether to deactivate the VNS device prior to surgery to prevent adverse events. Research suggests that VNS may increase vagal tone, which can affect cardiac rhythm during procedures (1).
Intraoperatively, management of the airway and cardiovascular system requires a multidisciplinary approach due to potential VNS-related complications. VNS can cause laryngopharyngeal dysfunction, which increases the risk of airway obstruction. Therefore, for safety reasons, tracheal intubation is generally considered a better choice than supraglottic airway devices when a patient undergoes surgery with an active vagal nerve stimulator (2). In addition, electromagnetic interference from surgical instruments, particularly diathermy, requires strict protocols to prevent inadvertent activation or damage to the VNS device. Surgeons and anesthesiologists must ensure that the diathermy path does not directly intersect the device or its leads. The use of tools such as bipolar diathermy minimizes interference and preserves the functionality of the VNS system.
The postoperative period requires careful monitoring and adjustment of the VNS device. If the device was deactivated preoperatively, reactivation should be planned in coordination with neurologists to align with the patient’s recovery. Depending on the patient’s postoperative neurological function and overall health, further adjustments to VNS settings may be necessary. Regular follow-up visits are critical to assess the effectiveness of these adjustments and to optimize VNS settings to ensure that the patient returns to or exceeds baseline neurological status (3).
In an emergency surgical setting, standard VNS management protocols may not always be applicable. Therefore, rapid decision-making and access to information are critical for the surgical team to quickly determine whether to deactivate the VNS device. Management strategies should remain flexible yet informed. Though time and information are limited in emergency surgery, clinicians should always prioritize patient safety and take reasonable precautions around a vagal nerve stimulator. In addition, physiologic responses to VNS may differ among pediatric, adult, and elderly patients, requiring specialized management strategies (1).
Effective management of VNS in the perioperative period is critical to the integration of VNS therapy into broader clinical practice. As the use of VNS increases, the development of refined perioperative protocols is essential to ensure patient safety and therapeutic efficacy. Future research should aim to optimize perioperative strategies and expand the evidence base to cover a wider range of surgical scenarios and patient populations, deepening our understanding of VNS interactions with various physiological systems during critical periods such as surgery. Ultimately, this approach will improve patient outcomes and ensure the therapeutic success of VNS.
References
- Morris GL 3rd, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy: report of the guideline development subcommittee of the American Academy of neurology. Epilepsy Curr. 2013;13(6):297-303. doi:10.5698/1535-7597-13.6.297
- Broderick L, Tuohy G, Solymos O, et al. Management of vagus nerve stimulation therapy in the peri-operative period: Guidelines from the Association of Anaesthetists: Guidelines from the Association of Anaesthetists. Anaesthesia. 2023;78(6):747-757. doi:10.1111/anae.16012
- Elliott RE, Morsi A, Tanweer O, et al. Efficacy of vagus nerve stimulation over time: review of 65 consecutive patients with treatment-resistant epilepsy treated with VNS > 10 years. Epilepsy Behav. 2011;20(3):478-483. doi:10.1016/j.yebeh.2010.12.042